Unraveling substrate recognition and transport by ATP binding cassette (ABC) transporters
ATP binding cassette (ABC) transporters are expressed in all phyla of life and constitute one of the largest protein superfamilies. They translocate very diverse substrates across cellular membranes at the expense of ATP hydrolysis. The best-investigated ABC transporter is P-glycoprotein (ABCB1, MDR1). It prevents drug and toxin uptake at absorptive membranes such as the intestinal (IB) and the blood-brain barrier (BBB), respectively, and enhances metabolite efflux at excretory barriers in proximal tubules of the kidney and biliary ducts of the liver. Cells can be induced to overexpress ABCB1 by the exposure to a single agent (e.g. anticancer drugs, certain antibiotics, or food components) or to physical stress, such as Xray, UV light irradiation or heat shock. Overexpression of ABCB1 leads to multidrug resistance (MDR), that is, to a resistance towards all drugs that are substrates forABCB1. The expression level of ABCB1 de pends (among other factors) on the exposure of cells to various stimuli. The same type of stimuli that induce MDR due to ABCB1 overe xpression in humans can also induce MDR in bacteria, parasites, and fungi by promoting the expression of related ABC transporters. MDR is detrimental not only for the treatment of many cancers, but also for the treatment of bacterial, parasitic, and fungal diseases and can be considered as a general problem for pharmacotherapy.
Although ABCB1 is known for more than 30 years, its substrate specificity and transport mechanism have long remained enigmatic. This is due on one hand to the unusual location of substrate binding site and on the other hand to the polyspecificity of the transporter. ABCB1 binds its substrates
in the cytosolic membrane leaflet and moves them to the extracellular membrane leaflet or directly to the extracellular medium, depending on the hydrophobicity of the substrate, quite in contrast most well characterized transporters that move substrates from the aqueous phase at one side of the membrane to the aqueous phase at the other side of the membrane. Substrate binding in the lipid membrane is thus preceded by a lipid-water partitioning step. We have shown that lipid-water partitioning is dominated by hydrophobic groups of the substrate, whereas substrate binding to the transporter in the lipid membrane is due exclusively to hydrogen bond acceptor groups of the substrate. To be transported by ABCB1 a compound has to carry minimally one binding module composed of two hydrogen bond acceptors. Up to ten binding modules have been observed whereby the binding affinity of the compound to the transporter in the lipid membrane increases linearly with the number of binding modules. Hydrogen bond acceptors recognized by ABCB1 are carbonyl, ether, or tertiary amino groups, halogen substituents and π-electron systems. The hydrogen bond acceptor groups in binding modules most likely form hydrogen bonds with the numerous hydrogen bond donor groups in the transmembrane domains of the transporter. In the lipid environment of the cytosolic membrane leaflet (exhibiting a low dielectric constant) hydrogen bonds are more specific and stronger than van der Waals interactions. As soon as the substrate reaches the extracellular leaflet, where water can approach, hydrogen bonds with the transporter vanish and the substrate is released either into the lipid or the aqueous phase.
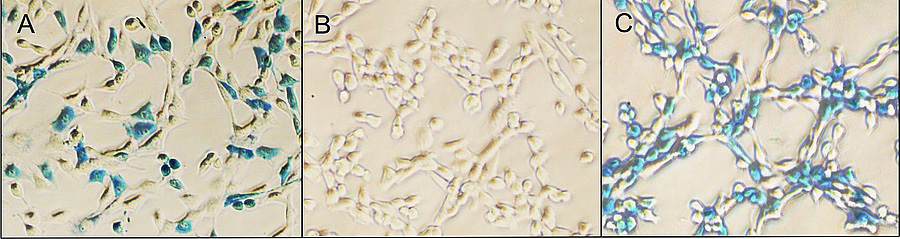
The rate of substrate transport by ABCB1 is directly proportional to the rate of ATP hydrolysis. However, the fact that substrates have to partition into the cytosolic membrane leaflet to bind to ABCB1 implies that many substrates partially escape to the cytosol before being caught by the transporter which complicates the analysis of substrate transport. Quantitatively comparing passive influx and active efflux of drugs revealed that the net flux of drugs across membranes protected by ABCB1 results from the sum of the two processes. For different compounds and a given membrane passive influx exponentially decreases with the size and the charge of the molecule and changes by several orders of magnitude for different compounds whereas active efflux is more constant and changes only by about one order of magnitude. Large and/or highly charged compounds diffuse slowly and are therefore prone to being completely effluxed by ABCB1. The diffusion step from the extracellular to the cytosolic leaflet is crucial for the fate of the molecule. If it is fast compared to efflux (flipping) compounds will reach the cytosol even though they are partially exported, however, if it is slow compounds will not reach the cytosol (see figure A-D). Our analyses revealed that the lipid bilayer membrane plays an important synergistic role in substrate binding as well as in substrate transport by ABCB1. By taking into account the membrane contribution allowed unraveling substrate recognition and transport by ABCB1. Ongoing projects in our laboratory are dedicated to elucidating the substrate specificity and function of other ABC transporters such as the Staphylococcus aureus transporter Sav1866, the cystic fibrosis transduction regulator (CFTR, ABCC7) and the cholesterol transporter ABCA1.